As it has been proved with the emergence of the COVID-19 virus, worldwide we are at risk of easily turning a local outbreak into a global pandemic. Two of the reasons for this are poor public healthcare and an inadequate healthcare infrastructure. Even developed economies, who do not suffer from either of these, are now facing increasing pressure on their national public health systems. One way through which international development can help to prevent and manage future possible pandemics is to direct more of its aid towards investments in public healthcare.
The US government’s Center for Disease Control and Prevention, one of the leading health organizations in the world, lists some of the main factors driving the risk of epidemic outbreaks occurring and rapidly spreading:
- Increased risk of infectious pathogens “spilling over” from animals to humans
- Development of antimicrobial resistance
- Spread of infectious diseases through global travel and trade
- Acts of bio-terrorism
- Weak public health infrastructures
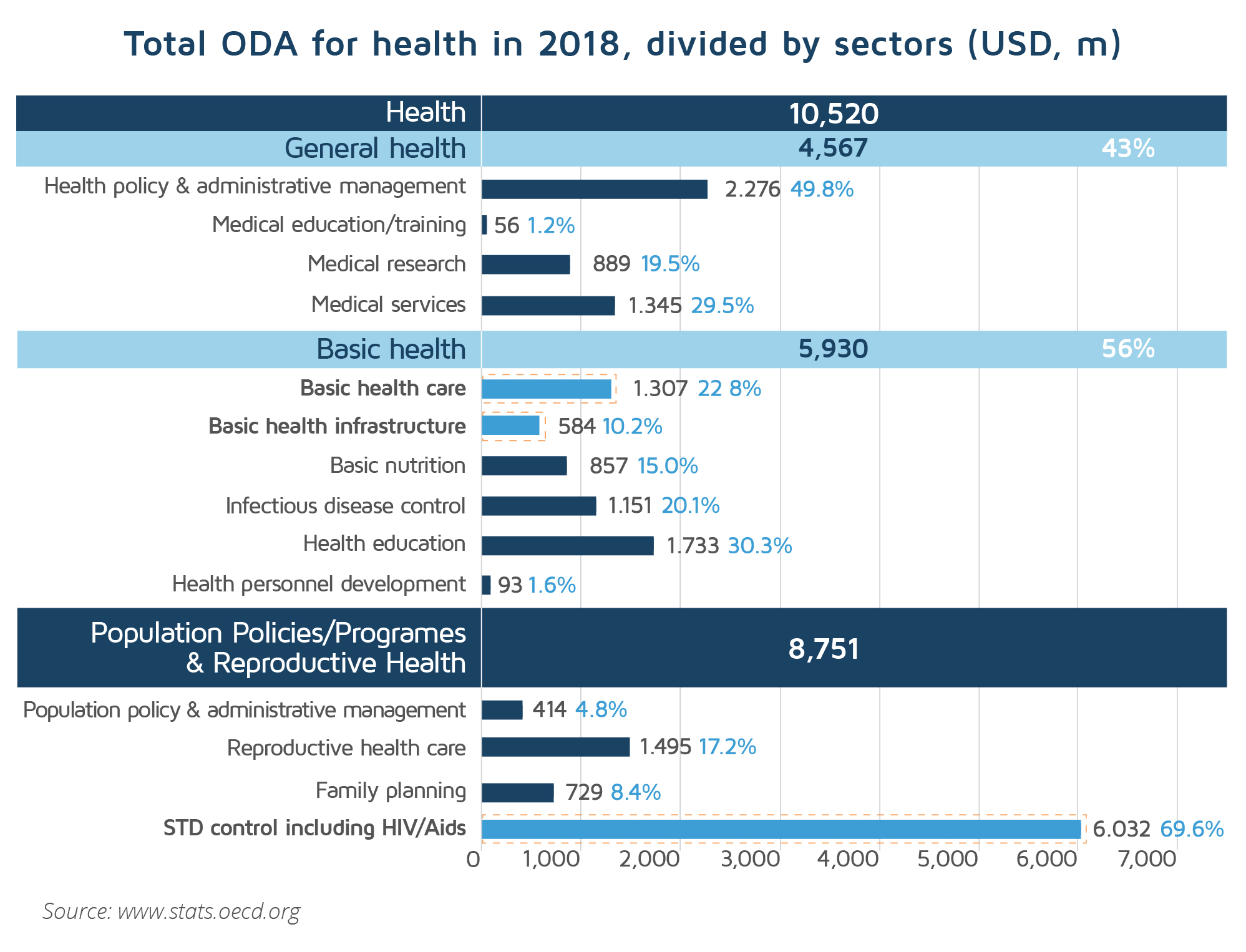
However, in international development, health spending trends have, for the last two decades, moved from broad systems-based investments to a more specialized, infectious disease model.
The growth of vertical, disease-specific global health programs has meant that the greatest growth in health aid funding has been related to the control of infectious diseases, particularly HIV/AIDS and malaria. This increasing trend has been evident since 2000, the launch year of the Millennium Development Goals (MDGs). According to the Organization for Economic Cooperation and Development (OECD), the percentage of health ODA allocated to infectious disease control aid (malaria, tuberculosis) has increased from 8% in the period 1990-1998 to 16% in the period of 2005-2008, while basic health infrastructure aid declined from 11% to 5% during 2005-2008. According to OECD data, in 2018 the largest share of global ODA, representing 57%, was allocated to HIV/AIDS control and only 12% and 5.5% were allocated to basic healthcare and healthcare infrastructure respectively.
Currently, pandemic prevention programs are most commonly funded through emergency or disaster relief mechanisms.
National public health systems are fundamental components of resistant health systems and the first line of defense against the threat of pandemic disease.
This means that only a functioning and resilient health care system with effective primary care delivery can withstand the test of epidemics. Primary care, as part of the healthcare system, is fundamentally patient-centered whereas public health focuses on population health. Both sets of capacities and infrastructure are necessary to prepare and respond to the threat of infectious diseases.
The importance of building strong public health systems was recognized globally following the SARS outbreak in 2002–2003 and avian influenza in 2003–2004. These outbreaks proved that regional and global capabilities cannot compensate for systemic deficiencies at national or local level. Moreover, overwhelmed health systems and other indirect effects may contribute to a 2.3-fold increase in all-cause mortality during pandemics. In a review study of nearly 400 public health events of international concern, the analysis showed that a breakdown or absence of public health infrastructure was the driving factor in the highest number of outbreaks (39.5%).
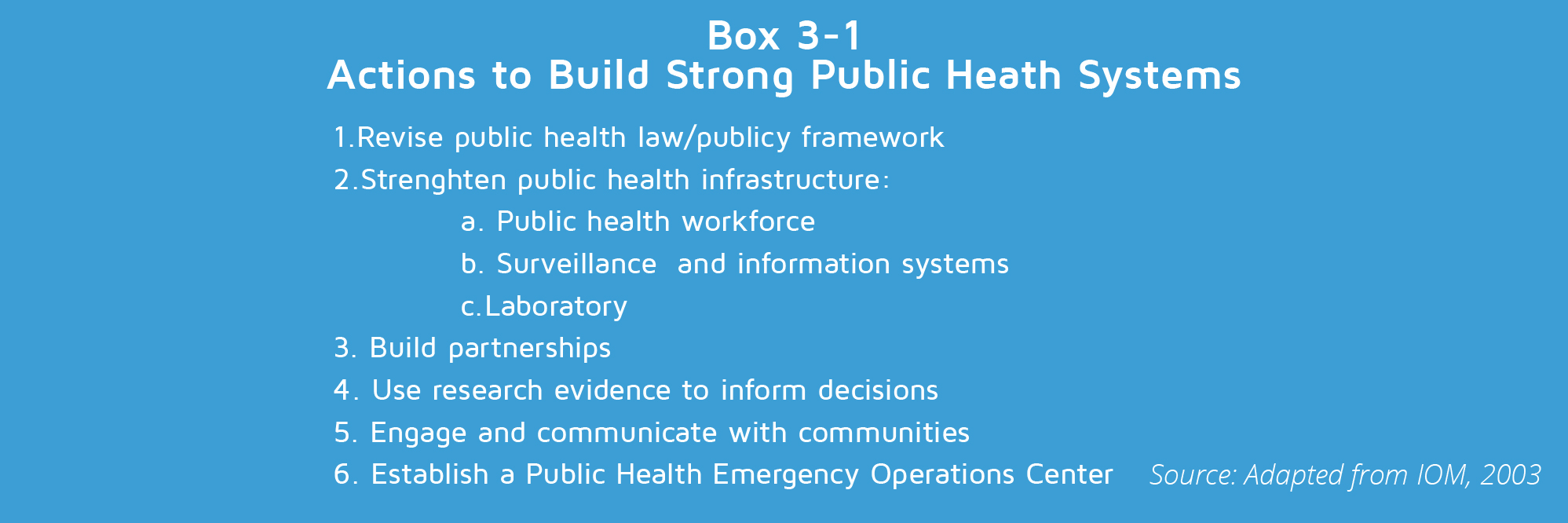
The most effective strategies for increasing pandemic preparedness, particularly in resource-constrained settings, consist of investments intended to strengthen the core public health infrastructure.
As the findings presented above show, establishing disease-specific global health programs may be at the cost of strengthening basic public health infrastructure in the long run. Accordingly, a long-term funding strategy that invests in a systematic and diagonal approach to strengthen national health systems would be more consistent with current developments.
To follow the latest developments related to the COVID-19 pandemic, become a member and register for our newsletter. You can also search through the current health funding opportunities listed on the DevelopmentAid platform.